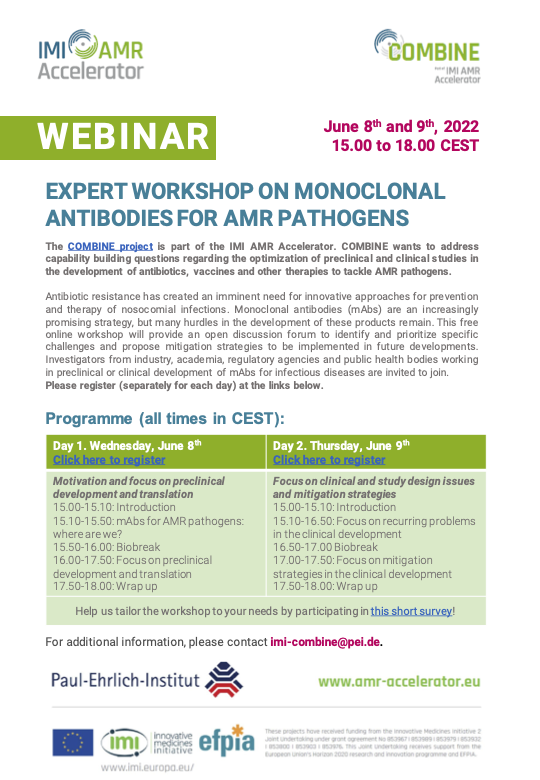
In June 2022, the Paul-Ehrlich-Institut organised a two-day virtual expert workshop on behalf of the COMBINE project. The workshop aimed to address the challenges in developing monoclonal antibodies (mAbs) against antimicrobial resistance (AMR) pathogens, with a specific focus on ESCAPE pathogens (E. faecium, S. aureus, C. difficile, A. baumannii, P. aeruginosa, and Enterobacteriaceae). The workshop brought together 24 experts from industry, academia, public health, and regulatory bodies to discuss recurring issues and potential mitigation strategies.
Experts highlighted the distinct challenges in developing mAbs for therapeutic or prophylactic treatments. Different approaches in designing mAb targets were discussed, including directly targeting the bacteria or targeting virulence factors. The importance of robust efficacy data from animal models before initiating clinical testing was emphasised. The potential use of Immunoglobulin M mAbs and inhalation administration for lung infections was also discussed. In the translational session, the experts discussed the integration of various variables into physiologically-based pharmacokinetic models, such as inflammation, tissue distribution, bacterial growth, and clinically relevant markers. The clinical session focused on the challenges in human drug development for mAbs, drawing learnings from COVID-19 trials. Experts highlighted the importance of selecting the right primary endpoint, identifying the appropriate patient population, and having rapid diagnostics available for future studies. Potential solutions to increase the efficiency of clinical trials were also discussed, including adaptive trials, clinical trial networks, and meta-analyses of smaller trials.
Overall, the workshop provided an open forum for experts to discuss and prioritise the challenges in the development of mAbs against AMR pathogens. The insights gained from the workshop will guide future work within the COMBINE project, aiming to overcome bottlenecks in the preclinical and clinical development of mAbs against AMR. This is particularly important given the promising potential of mAbs in treating and preventing AMR infections, particularly those caused by ESCAPE pathogens.



